Welcome To Our Blog!
Welcome to the Cary Eye Center Blog. stay Tuned for new posts and the latest news!
There are some exciting, new developments in Dry Eye Disease. Many patients do not know that they even have this condition until they go to their eye doctor and get a thorough examination. The medical term for Dry Eye Disease is Keratoconjunctivitis Sicca. If you have any of the following symptoms, you may have Dry Eye:
Many patients have Dry Eye. There may be a genetic predisposition to having it, but some common risk factors for developing Dry Eye Disease include:
Findings in Dry Eye: The front surface of the eye, called the cornea, is primarily affected in Dry Eye. A normal or healthy eye would have a smooth, clear surface (Fig. 1).

Figure 1
In contrast, an eye with Dry Eye Disease shows an irregular surface with a scattered light reflection and, in severe cases, may have stuck on pieces of mucus (Fig. 2).

Figure 2
One of the most useful tests for doctors in evaluating for Dry Eye is to stain the cornea with fluorescein. Once again, instead of a smooth, even surface, the stain will reveal many irregular areas and erosions in the corneal epithelium (the surface layer) (Fig. 3).
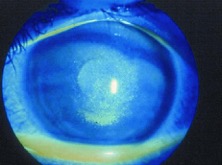
Figure 3
Treament for Dry Eye usually starts with Over-The-Counter remedies, such as lubricating eye drops (called Artificial Tears) or lubricating ointments. For some patients, dietary items may help such as Fish Oil and Flaxseed Oil. This may help patients who have mild Dry Eye. Contact Lens wear can make Dry Eye worse and often non-prescription rewetting drops or preservative-free Artificial Tears can be used successfully. However, lubrication for many patients only provides short-term relief (30 minutes) and more treatment is warranted.
Another older treatment for Dry Eye involves blocking the outflow of tears at the level of the punctae, the small holes on the inner side of the eyelids that drain tears through the lacrimal system and into the nose and back of the throat. This is called punctal occlusion. A silicone punctal plug is seen inserted into the lower eyelid in Fig. 4. In theory, this procedure keeps more tears in the eye and improves comfort. In practice in is helpful for some patients.

Figure 4
Medical treatment for Dry Eye primarily involves anti-inflammatory drops, as Dry Eye Disease is generally understood in terms of being an inflammatory condition. This condition can both reduce the amount of tears produced (Aqueous Tear Deficiency), the quality of the tears produced, and/or the reduction of the tear film through evaporation due to a poor quality of the oil layer that rides on top of the tear film (Evaporative Tear Deficiency). This cycle of inflammation is diagrammed in Fig. 5:
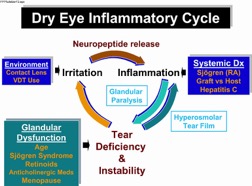
Figure 5
For short-term treatment, steroid drops are often used. These medications contain corticosteroids which reduce inflammation and can rapidly improve the symptoms of Dry Eye. However, these treatments must be monitored carefully as steroids have known side effects in the eye. This treatment approach might include such drops as Pred Forte, prednisolone acetate, Alrex, and Lotemax. Excessive use of steroid drops, however, may cause a progression in cataracts or an increase in the intraocular pressure, which can cause glaucoma.
For long-term treatment of well-documented Dry Eye, there are now two prescription medications that are not steroids that can reduce inflammation and are approved for the treatment of Dry Eye by the Food & Drug Administration. The first medication, which has been available by prescription since 2003, is Restasis (cyclosporine). The chemical structure of cyclosporine is shown in Fig. 6:
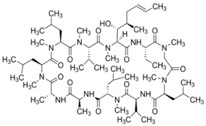
Figure 6
Restasis is very helpful for most patients that try it. One drawback is that it can take several months to begin to ease the symptoms of Dry Eye. In fact, it has been shown to be increasingly helpful as the time of use increases from 2 to up to 6 months. It does not have any of the side effects of steroids. In some patients, however, it may cause burning or redness.
The newest prescription treatment for Dry Eye was just released in August, 2016. It is called Xiidra (lifitegrast). The structure of lifitegrast is shown in Fig. 7.
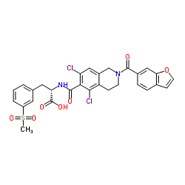
Figure 7
This is an exciting development for patients with Dry Eye. Xiidra works as an anti-inflammatory in a novel way, which involves inhibiting immune cells (T cells) through molecules on their surfaces called LFA-1 and ICAM-1. This new drop also takes time to have its effect on the eye and may take up to 6 weeks or more to show an improvement in symptoms. Our own clinical experience with Xiidra at Cary Eye Center is limited because the drug was just approved for release. Like any eye drop, it may cause some burning or irritation and can cause some change in the sense of taste, called dysgeusia, as was noted in the FDA trials.
Conclusion: Dry Eye Disease is fairly common and can be treated by multiple treatment approaches, many of which are reviewed above. Some of these treatments can be used in combination to optimize their effects and provide the best possible comfort for patients that suffer with this condition.
Figures 2-5, © 2016 American Academy of Ophthalmology